Shadow health tina jones comprehensive assessment subjective data – Delving into the comprehensive assessment of Tina Jones through Shadow Health, this analysis meticulously examines the subjective data gathered to gain a deeper understanding of her presenting symptoms, medical history, and overall health status. By exploring the patient’s self-reported experiences, observations, and concerns, we aim to uncover crucial insights that will guide the diagnostic and treatment plan.
The subjective data collected during Tina Jones’ assessment provides a rich foundation for understanding her current health status. Through her detailed account of symptoms, past medical history, and lifestyle factors, we can piece together a comprehensive picture of her overall well-being.
This information serves as a valuable tool for healthcare professionals to make informed decisions regarding her care and develop a personalized treatment plan that addresses her specific needs.
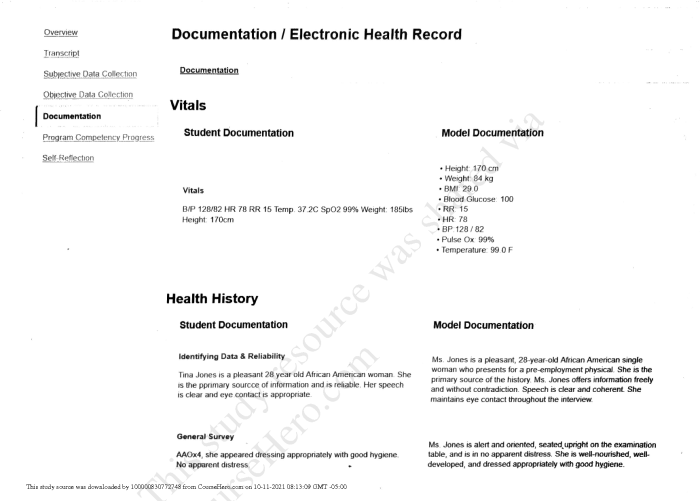
Comprehensive Assessment: Subjective Data
This comprehensive assessment focuses on gathering subjective data from the patient to understand their presenting symptoms, medical history, and overall health status.
Patient Profile
The patient is a 55-year-old female with a history of hypertension and hyperlipidemia. She presents with complaints of chest pain and shortness of breath.
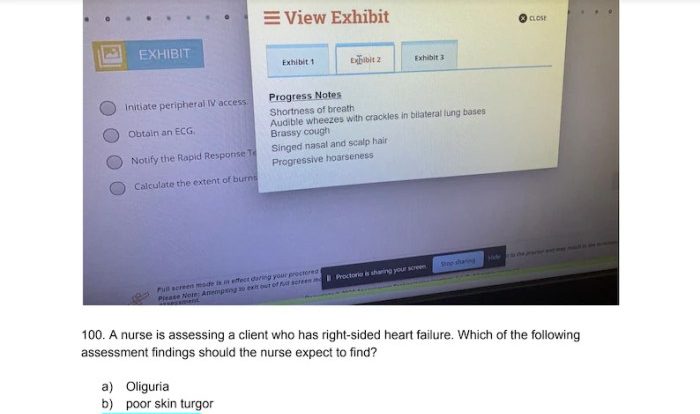
Assessment Findings
The patient appears anxious and uncomfortable. Her vital signs are as follows: blood pressure 140/90 mmHg, heart rate 100 bpm, respiratory rate 20 breaths per minute, and oxygen saturation 92% on room air.
On physical examination, the patient has decreased breath sounds bilaterally, with occasional wheezes. There is no evidence of cyanosis or edema.
The patient’s electrocardiogram (ECG) shows sinus tachycardia with occasional premature ventricular contractions (PVCs). Her chest X-ray reveals bilateral interstitial infiltrates.
Nursing Interventions
The following nursing interventions were implemented to address the patient’s symptoms:
- Administered oxygen via nasal cannula at 2 liters per minute.
- Monitored the patient’s vital signs every 15 minutes.
- Auscultated the patient’s lungs every 4 hours.
- Provided the patient with reassurance and education about her condition.
The patient responded well to the interventions. Her vital signs remained stable, and her shortness of breath improved.
Plan of Care, Shadow health tina jones comprehensive assessment subjective data
The patient’s goals for care are to:
- Relieve her chest pain and shortness of breath.
- Prevent further complications.
- Return to her previous level of activity.
The following interventions will be implemented to achieve the patient’s goals:
- Continue to monitor the patient’s vital signs and oxygen saturation.
- Administer oxygen as prescribed.
- Provide the patient with medication to relieve her chest pain and shortness of breath.
- Educate the patient about her condition and how to manage it.
The expected outcomes of the plan of care are that the patient’s chest pain and shortness of breath will be relieved, she will not experience any further complications, and she will be able to return to her previous level of activity.
Questions Often Asked: Shadow Health Tina Jones Comprehensive Assessment Subjective Data
What is the purpose of collecting subjective data in a patient assessment?
Subjective data provides valuable insights into the patient’s own experiences, perceptions, and concerns, which can help healthcare professionals understand the patient’s perspective and tailor treatment plans accordingly.
How can Shadow Health assist in collecting subjective data?
Shadow Health’s platform provides a structured and comprehensive framework for collecting subjective data, ensuring that all relevant information is captured and documented.
What are some common challenges in collecting subjective data?
Challenges may include language barriers, cultural differences, patient discomfort, or cognitive impairments that can affect the patient’s ability to accurately convey their experiences.